Tuesday, July 25, 2006
Some Male Reproduction and Female Reproduction
(Contributed by Nancy Rumore)
Erection: psychic turns on Parasympathetic – smooth muscle relaxes and blood flows into vessels
Emission: encouragement Sympathetic causes peristalsis
Ejaculation: spinal cord reflex triggered by semen entering the prostatic urethra
Produce 3.5 ml per ejaculate
120 million sperm/ml
Corpora cavernosa – make up most of the penis and are bound by fibrous tunica albuginea
Space for drawing
Corpus spongiosum – surrounds the urethra and forms the bulb of the penis
When flaccid, the smooth muscles in the penis are constricted
FEMALE REPRODUCTION
Ovaries – female gonads
Two purposes: produce gametes and hormones
Hormones: progesterone and estrogen
Accessory ducts are: uterine tubes, uterus and vagina
OVARIES
Ovaries are served by ovarian arteries-branches of abdominal aorta and ovarian branch of uterine arteries
Ovaries are surrounded by tunica albuginea which is surrounded by germinal epithelium.
The ovary has a cortex where the oogonia are housed. (millions of oogonia- most immature sex cell)
The medulla in the ovary is where the blood vessels are.
In the female fetus, the oogonnia undergo mitosis, enter a growth phase and lay in nutrient reserves.
The female baby is born with primary oocytes (46 chromosomes). There are 7 million of these.
These primary oocytes are embedded in stroma and are surrounded with follicle cells. This is the primordial follicle.
At puberty, 700,000 oocytes remain. GH plays a big role in getting to puberty.
Ovarian cycle 1-28 days
Day 1 -10
Hypothalamus releases FSHRH and LHRH
Goes to the ant pit gland which releases FSH and LH
FSH “picks” 25 primordial follicles and tells them to mature. FSH attaches to the cells on the follicles and tell them to make estrogen.
The follicle cells take on the name granulose cells. The primordial follicle becomes the primary follicle when the follicle matures and the oocyte grows. Some of the oocytes die along the way.
A layer of connective tissue surrounds the follicle called the theca folliculi. Theca and granulose cells produce estrogens with some of the theca cells making androgens (converted to estrogen along the way).
The granulosum cells will secrete a thick transparent membrane called the zona pellucida around the oocyte. A clear liquid will accumulate between the granulose cells called antrum. The primary follicle is now a secondary follicle.
Because Inhibin is released by the granulose cells exhibiting negative feedback on FSH and LH because the estrogen levels are rising. LH and FSH levels drop.
Day 10-13 Graffian follicle (mature follicle)
When estrogen levels are very high, there is positive feedback on FSH and LH causing their levels to surge, mostly LH levels.
LH does two things: causse the primary oocyte of the dominant follicle to form a polar body (secondary oocyte) and causes tunica albuginea to thin and rupture. Day 14
Day 14- 28 The theca caves in and grows. It now transforms into the corpus luteum (CL). The secondary ooccyte is now encased in corona rediata (no longer granulosa cells)
Other follicles are absorbed.
The corpus luteum (CL) becomes an endocrine gland secreting progesterone and some estrogen. If pregnancy does not occur, the CL will degenerate in about ten days and a white scar will form (corpus albicans). If pregnancy occurs, the CL will continue to secrete progesterone until the placenta takes over in three months.
The secondary oocyte sill move into the uterine tube where in the upper 1/3 of the tube is where fertilization begins.
The Menstrual cycle
Days 1 – 5 Menstrual phase
Shedding of endomentrium (doesn’t shed its deepest part, however)
FHS and LH are low; estrogen and progesterone are also low
Day 5
Follicles are beginning to produce estrogen so these levels rise, progesterone is still low,
Day 6-14 Proliferative phase
Endometrium rebuilds itself, thickening and engorged with blood. Progesterone receptors are being synthesized. Cervical mucus becomes thin.
Ovulation occurs – LH levels are high, FSH levels are higher here, estrogen is at peak, then drops as progesterone levels increase. Ruptured follicle converts to CL.
Day 15 – 28 Secondary Phase
Endometrium prepares for implantation of fertilized egg. Progesterone levels are soaring. Uterine glands enlarge and secrete glycogen into the uterine cavity. The cervix mucus becomes thick.
LH is inhibited.
If no pregnancy occurs, the CL disintegrates and the progesterone levels fall, the endometrium sloughs off, lysosomes of endometrial cells rupture, functional layers self digest and a period begins.
Estrogen promotes fat deposits, growth of breasts, widening of pelvis, feminizing the body, growth of pubic hair, mainitain low blood cholesterol levels, facilitating Ca2+ uptake (bone density)
Progesterone works with estrogen to regulate the uterine cycle, promote changes in cervical mucus, lactation in the breasts
During pregnancy, the main source of estrogen and progesterone is the placenta.
Monday, July 24, 2006
Male reproduction and sperm illustration
Sexual Reproduction (submitted by Nancy Rumore)
Males
 Sperm Illustration below
Sperm Illustration belowTestes – male gonads that lie in the scrotum
In embryonic development, the testes in in the body are found in germinal epithelium. Before birth, they descend to the scrotum through the inguinal canal. They are pulled down by the gubernacerlum to the scrotum.
Testes form because of presence of testosterone. The testes are encapsulated in tunica albuginine
There are two major parts of the testicles:
1) Testes where you will find the Seminiferous tubular part
2) Epididymis part
Path of sperm:
Seminiferous tubules is where sperm is made. Inside these tubules are Nurse (Sertole or Sustemtacular) cells. These cells nourish and push along the spermatogonia.
The seminiferous tubule:
a) join to form a straight tubule called a tubulus rectus
that
b) sends sperm into the rete testis to the efferent ductules
c) to the epididymis
d) to the ductus epididymis
e) to the vas deferens or spermatic cord.
f) sperm travels to the ampulla of the vas deferens
g) to the ejaculatory duct which is surrounded by the prostate. The prostate gland releases milky, white fluid (1/3) of semen volume.
h) The bulbourethal gland secretes a clear mucus that neutralizes urine in the urethra.
i) The seminal vesicles, located on the posterior of the bladder, secrete 60% of the seminal fluid, an alkaline based mixture.
In the spermatic cord, there are:
1) capillaries
2) lymphatic vessels
3) nerve cells
The cremaster muscle holds the testicle in place and brings it up toward the body when it is cold outside (lowers testes when it is hot). The testes must be kept cool in a hot environment and warm in a cold environment.
The prostate gland contracts muscle during ejaculation
Urethra
Conveys semen and urine.
Three regions:
1) prostatic urethra – surrounds the prostate gland - 1 - 1.5 inch
2) membraneous urethra
3) spongy penile urethra - six inches (if they are lucky) (just a joke)
Interstitial cells of Leydig make testosterone.
FSH goes to the semiferous tubules to tell them to make sperm
Penis
With the scrotum, part of the external genitalia and hang from the perineum
Penis has an attached root, shaft and the glans penis.
Corpus spongiosum surrounds the urethra and goes all the way to the root where it is called the bulb of the penis.
Production of sperm
Spermatogenesis is the formation of sperm
Website: http://www.cvm.okstate.edu/instruction/mm_curr/histology/MR/HiMRP4.htm
This website speaks at length about sperm formation
Spermatid now in the coils
-has to get excess cytoplasm removed
-undergoes huge metabolism
-acidity keeps it from moving
-don’t have to waste energy
-bulbourethral gland helps spermatids move by secreting fluid into the urethra, reducing the acidity
Kidneys-filtration, reabsorption, secretion
-are retroperitoneal in superior lumbar region
-consists of a renal fascia, adipose capsule and renal capsule (from outside in)
-has a superficial cortex, medulla with pyramids, and medial pelvis
-receive 25% of total cardiac output/minute
Kidney (renal) functions:
1) gluconogenesis during prolonged fasting
2) produce rennin which regulates BP and kidney function
3) produce EPO which stimulates RBC production
4) metabolizing vit D to active form
Adrenal gland sits on top of each kidney
The ureters, renal blood vessels, lymphatics and nerves all join the kidney at the renal hilus which leads into the renal sinuses.
The apex of the pyramids are the papilla which means nipple – contain bundles of collecting tubules (inside the pyramids).
Columns separate the pyramids
Seven lobes of a kidney
Major calyx and minor calyx are where urine is collected and is emptied into the renal pelvis which goes to the ureter to the bladder.
Know drawing and the movement into and out of the kidneys
No lobar or segmented veins in the kidneys
Renal plexus is a network of nerve fibers and ganglia and is supplied by the parasympathetic fibers from the 12th thoracic and the 1st lumber splanchic nerves
Nephrons
-consists of a glomerulus and renal tubule (glomerular capsule (Bowman’s capsule), PCT, loop of Henle, DCT) Peritubular capillary is associated with the renal tubule of each nephron.
PCTThere are microvilli (Brush Border) in the PCT and cubodial cells. And many mitochondria. Reabsorb nutrients and water.
Descending limb of the loop of Henle-thin segment-permeable to water
Ascending limb of the loop of Henle-thick segment
DCT
Cells are cubodial but are thinner and no microvilli
Secrete solutes into filtrate rather than reabsorb as much
Toward the collecting tubule, the DCT becomes more like the collecting tubules
Intercalated cells, cubodial cells w/microvilli and principal cells
Intercalated cells maintain acid-base balance of blood
Principle cells maintain body water and Na+ balance.
Cortical nephrons – 85% of nephrons in kidney-located in the cortex
Juxtamedullary nephrons – 15% of nephrons in kidney-located close to cortex-medulla junction – produce concentrated urine
-Vasa recta-capillaries that supply loop of Henle in the medulla region of the kidney
Nephron Capillary Beds --Glomerulus and Peritubular capillaries
Glomerulus –specialized for filtration
Afferent arterioles-high BP, larger diameter, forces fluids and solutes into glomerulus
Efferent arterioles-break into the peritubular capillaries,
low BP, fenestrated capillaries, absorb solutes and water from the tubule cells from the filtrate and return to blood in the peritubular capillary beds
Efferent arterioles serving the juxtamedullary nephrons do not break into the peritubular capillaries-form bundles of long straight vessels called Vasa recta-form concentrated urine
Renal BP goes from 85 mg in the renal arteries to 8 mg in the renal veins Net filtration pressure is 10 mg.
Efferent arterioles-peritubular capillaries
Juxtaglomerlar cells – acts as mechanoreceptors that send BP in the afferent arterioles in the arteriole walls
Macula densa-group of closely packed DCT cells that respond to changes in the solute content of the filtrate.
These two groups of cells regulate rate of filtrate formation and systemic BP
Filtration Membrane-allows for free passage of water and solutes
Layers: 1) fenestrated epithelium of glomerular capillaries-allows passage of plasma components but not blood
2) visceral memberane in glomerular capsule of PODOCYTES
3) basement membrane
Three major mechanisms by which the kidneys adjust plasma composition:
1) glomerular filtration
2) tubular reabsorption
3) tubular secretion
Glomerular Filtration: Filtrate and urine: filtrate contains everything in blood plasma except proteins Urine is mostly metabolic wastes Kidneys produce 180 liters of filtrate per day Plasma Proteins and blood cells stay in the capillaries
Tubular reabsorption Glucose and AA are reabsorbed (passively or actively)
PCT – absorbs Na+, all nutrients (glucose, AA K+, Ca2+, Mg2+), Cl-, H20, urea and lipid-soluble solutes, small proteins
(active transport with Na+, passive transport with Cations, osmosis with H2O, passive diffusion with urea and lipid-soluble solutes
Loop of Henle – absorbs H20, Na+, Cl-, K+ Ca2+, Mg2+
DCT – absorbs Na+, Ca2+, Cl-, H2O
(active transport with aldosterone for the Na+ ion, diffusion and osmosis)
Collecting duct –absorbs all of the above (DCT) plus urea
Tubular secretion; As the blood becomes more acidic, the renal tubule cells secrete more H+ into the filtrate and retain more HCO3- and K+ and H+ goes into the urine
As blood becomes more alkaline, the renal tubule cells will absorb more Cl- and HCO3- is secreted into the urine.
Both of these result in the regulation of blood pH.
Osmolarity-
Loop of Henle – descending limb is impermeable to solutes and permeable to water. Water is reabsorbed thru the descending limb
Ascending limb is impermeable to water but permeable to salt. NaCl is reabsorbed into the ascending loop of Henle. The use of co-transport occurs here (co-transport = picks up Na+ and a glucose comes with it) (active transport with pumper)
Albumin in filtrate -DON”T WANT THIS may find albumin in urine in pregnant women and when BP is high during vigorous exercise
Urea is a useless waste product but 50% diffused back into blood as a standard for negative feedback system(passive transport)
Uric acid (is a useless substance but retrieve 90% back into blood (active transport
Aldosterone regulates Na+ and tells K+ to get out
Parathormone regulates PO4 H+ combines with PO4 to become H2PO4
This gets H+ out of the PCT regulates pH of blood
Acidosis – H+ ions are produced by the body- more acidic blood (Bohr Effect- O2 less likely to jump off Hb) pH drops too much – you pickle
ADH release from supra optic release a lot of ADH – urine becomes concentrated
Release a little ADH, the urine becomes diluted
Diuretics include the following: Lasix or other types of diuretic drugs, caffeine-based drinks like coffee, tea, and colas, and alcohol
Normal Urine contains the following:
Urea, uric acid, creatine, Na+, K+, PO4, SO4
The bladder
Has three layers: mucosa epithelium, muscular layer called the detrusor muscle, and the fibrous adventitia layer. The smooth triangular area is called the trigone and this is where most infections occur (at the base of the bladder)
Bladder contains rugae and can stretch.
Urethra
Thickening of the detrusor muscle forms the internal urethral sphincter which keeps the urine in.
The external urethral sphincter is skeletal muscle and is voluntary
Male urethra carries urine and semen out
Micturition = urination
Because the external sphincter muscle is voluntarily controlled, micturition can be delayed temporarily.
Gather 125 mg of filtrate/minute but only collect 1-3 mg /minute for excretion
Kidney link
This site has several illustrations that are very helpful when it comes to trying to understand the kidney.
Saturday, July 22, 2006
Heart
Heart weighs about 250 – 350 grams
Heart is a transport system pump using blood as a transport medium
Located in the mediastinum – medial cavity of the thorax
Point of maximal intensity is where you press your finger between the fifth and sixth rib, where the apex contacts the chest wall
Pericardium – double walled sac the encloses the heart
Fibrous pericardium – loose fitting superficial part of the pericardial Sac
Serous pericardium – thin slippery two layer serous membrane- parietal layer and visceral layer (also called the epicardium layer)
Inflammation of the pericardium – Pericarditis
Layers of the Heart:
Epicardium
Mycocardium
Endocardium
Atria
Ventricles
Interatrial septum
Interventricular septum
Coronary sinus
Superior and inferior vena cava
Four pulmonary veins enter the left atria from the lungs
Papillary muscles play a role in value function
Look at diagram on page 682 in textbook for circulatory system
Pulmonary circuit – blood vessels that carry blood to and from the lungs
Systemic circuit – blood vessels that carry the functional blood supply to and from all body tissues
Right side of the heart is the pulmonary circuit pump
Left side of heart is the systemic circuit pump
Coronary circulation is the functional supply of blood to the heart
(Know the parts of the heart)
Cardiac muscle is striated and contract by the sliding filament mechanism
Cardiac cells are short, fat and interconnected and has centrally located nuclei
Intracellular spaces of the Cardiac muscle contains CT matrix filled with capillaries
Intercalated discs contain desmosones and gap junctions
Cardiac muscle has a lot of mitochondria organelles which give cardiac muscle the ability to resist fatigue. The heart requires more O2 for its energy metabolism than does skeletal muscle.
Some cardiac muscle cells are self excitable and can initiate their own depolarization in a rhythmic way – Autorhythmicity
The heart contracts as a unit due to depolarization waves across gap junctions
Na+ channels are open longer in cardiac muscle – absolute refractory period explains why heart muscles are protected against tetanus
Na+ channels are opened during depolarization causing an AP
The depolarization wave causes the sacroplasmic reticulum to release Ca2+ ions which cause the myofilaments to sliding across themselves (actin and tropin)
The time that Ca2+ channels stays open helps to explain why the AP and contractile phase is so much longer in cardiac muscle than in skeletal muscle. This helps in the heart ejecting blood from its chambers.
Ischemic – when the heart is deprived of blood, the cells are starving for oxygen and begin to metabolize anaerobically making lactic acid. The rise in H+ hinders the cardiac cells ability to produce ATP which is needed for Ca2+ channel pumps to open into extracellular fluid. When you have an increase in H+ and Ca2+ levels, the gap junctions will close, bypassing the damaged cells and forcing AP to go elsewhere…heart attack.
Independent but coordinated activity of the heart is a function of:
1) presence of gap junctions
2) intrinsic cardiac conduction system –initiates and distributes impulses throughout the heart so that it beats in a coordinated fashion
(There is a section on autorythmic cells and AP on page 690 that is rather detailed that you might want to look at)
Autorythmic cells are found in the following:
1) SA node – pacemaker
2) AV node – above tricuspid valve
3) Bundle of HIS
4) Left and right bundle branches
5) Perkinje fibers which supply the papillary muscles and are more prominent on the left side of the heart
The cardiac centers are located in the medulla oblongata
EKG or ECG is a composite of all AP generated by nodal and contractile cells
Deflection waves are the following:
1) P wave – lasts about 0.08 sec and results from the depolarization wave from the SA node to the atria
2) QRS complex – results from ventricular depolarization and precedes ventricular contraction.
3) T wave is caused by ventricular repolarization and last 0.16 sec
Heart murmurs are do to thin heart walls, defective values.
Systole – contraction period
Diastole-relaxation period
Cardiac output – amount of blood pumped out by each ventricle per minute (70 ml x number of beats per minute (75, 72 )
Stroke volume is the volume of blood pumped out of heart per minute (70 ml)Starling Law of the Heart – check handout
Tachycardia – fast heartbeat
Bradycardia – slow heartbeat
If the left side of the heart fails – pulmonary congestion occurs-edema in lungs
If the right side of the heart fails, peripheral congestion-edema in body, most noticeable the ankles, feet and hands
Thursday, July 20, 2006
Blood worksheet
1. Blood
Connective tissue
Formed elements suspended in plasma (nonliving fluid matrix)
Spin blood in a centrifuge:
Erythrocytes 45% of total volume of blood HEMOCRIT
aka RBC transports O2
Leukocytes aka WBC protects the body
Platelets stops bleeding
Both only make up 1% of total volume of blood
Also called BUFFY COAT
Plasma makes up remaining 55% of blood
Blood pH is 7.35 – 7.45
Five times thicker than water
8% of body weight
5 – 6 liters of blood in body
5 for females 6 for guys
Purposes:
Delivers O2 and nutrients
Transports wastes
Transports hormones
Regulates body temp by absorbing heat and distributing heat
Maintain pH
Maintains fluid volume
Platelets and plasma proteins form clots to prevent blood loss
Prevents infection with WBC, antibodies, etc
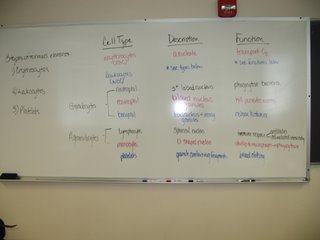
Blood and its elements
1) RBC -Erythrocytes – erythrocyte cells – anucleate – transport O2
2) WBC – Lymphocytes –leukocyte cells – Granulocytes
Granulocytes: a) Neutrophil – phagocytose bacteria
b) Eosinphil – kills parastic worms
c) Basophil – releases histamines
3) Platelets –Agranulocytes
a) Lymphocytes – B-cells, T-cells – immune response
b)Monocytes – become macrophages- phagocytosis
Platelets – blood clotting
RBC production
Formed in yolk sac, liver. Spleen in embryo
Formed in vascular sinuses of red bone marrow in adults
Hemocytoblast (stem cell)- has nucleus but cannot make Hemoglobin
How RBC cells are formed: ERYTHROPOIESIS
Stages of RBC formation: Hemocytoblast – Proerythroblast-early erythroblast – late erythroblast-normoblast (hemoglobin accumulation) -reticulocyte (ejection of nucleus) - erythrocyte
EPO is a glycoprotein hormone that stimulates the production or erythrocyte production
Produced by liver and mostly by kidneys
When kidney cells become hypoxic (need O2) -accelerates release of EPO.
EPO formation is triggered by:
drop in # of RBC due to hemorrhage or RBC destruction
reduced O2 available
exercise
EPO in blood causes hemocytoblasts to mature into erythrocytes faster
Testosterone also increases EPO production by kidneys
Chemicals released by leukocytes, platelets and
reticular cells stimulate EPO production
RBC destruction
RBC lasts about 120 days – go to spleen “red blood cell graveyard” removed by macrophages
Hemoglobin is split up into HEME and GLOBIN
Iron in Heme binds to a protein and is stored
The rest of heme is degraded to bilirubin, yellow pigment, bound to albumin. Sent to intestine where it is metabolized to urobilinogen, is sent out of body in feces as a brown pigmented sterocobilin (Textbook explanation)
As shown in handout, Iron in Heme breaks down to iron and biliverdin (which is converted to bilirubin and removed from body in bile salts)
Iron goes to bone marrow and is reused
1/15 of RBC removed everyday
Erythrocyte Disorders
Anemia
Insufficient no. of RBC due to hemorrahaging, rupture of erythrocytes, destruction of red bone marrow
Low hemoglobin content
Iron deficiency, deficiency of Vit B12
Abnormal hemoglobin - Sickle cell, thalassemia
Polycythemia- Excess erythrocytes –sluggish blood
WBC Production
The only formed elements that are complete cells with nuclei and organelles.
Account for only 1% of total blood volume.
Less numerous than RBC
Crucial to our defense against disease, bacteria, viruses, parasites, toxins and tumor cells
RBC are confined to bloodstream, while WBC can slip in and out of the capillary blood vessels
Two major categories:
Granulocytes – neutrophils, basophils, and eosinphils
Mostly neutrophils
Agranulocytes – lymphocytes (T and B cells),monocytes (macrophages)
Leukocyte disorders – leukemias, mononucleosis
Platelets are not cells in the strict sense. They are cytoplasmic fragments of extraordinary large cells.
They are essential for clotting where blood vessels or ruptured. They age quickly and degenerate in 10 days if not involved in clotting.
Vessels constrict accelerating coagulation
Prothrombin with Ca and phospholipids converts to thrombin (enzyme)
Thrombin cataylyzes the joining of fibrinogen molecules to become fibrin mesh which traps blood cells and seals the hole.
Prothrombin and fibrinogen are proteins formed by liver
Vit K is essential in making the liver synthesize prothrombin
BLOOD PLASMA
All formed elements removed – straw colored
92% water
Proteins 7% of plasma
Albumines – 60% of proteins – liver produces
Globulins – 36% of proteins Alpha and Beta transport lipids and are made by liver
Fibrinogen – 4% of proteins – made by liver
Non-protein substances – urea, uric acid, creatine, creatinin
Nutrients
Regulatory substances (hormones, enymes)
Resp gases
Electrolytes
Blood is classified as CT because it satisfies the requirement that it transports substances in the body.
2.Arteries, Veins and Capillaries
Arteries carry blood away from the heart (oxygenated)
Veins carry blood to the heart (deoxygenated or dirty blood)
Blood that travels from the heart thru arteries goes to arterioles (little arteries) that feed into capillary beds of tissues and organs
Blood drains from the capillaries into venules (smallest veins)
The blood from venules go to larger veins that eventually go back to the heart
Blood vessel walls have three layers called tunics
1)Tunica interna or tunica intima is the innermost layer
contains endothelium (simple squamous epithelium) that is a continuation of the endocardial lining of the heart.
2)tunica media is circulary arranged smooth muscle cells and sheets of elastin which is regulated by vasomotor nerve (vasodilation or vasoconstriction occurs here)
3)tunica externa or adventitia is loosely woven collagen fibers that protect the vessel contains nerve fibers, lymphatic vessels and elastin fibers
Tunica media is thick in arteries and thin in veins
Tunica externa is thin in arteries and thick in veins
Capillaries have only the endothelium and sparse basal lamina
They are the smallest blood vessels
Arteriosclerosis narrows arteries and thickens the walls of the arteries
The aorta and coronary arteries are most often affected
It is caused by a variety of things: bacterial infections, viral infections, hypertension, poisons like arsenic, most likely plaque which seems to injure the endothelial cells. When plaque nicks the cells, they repair themselves by depositing all kinds of things like LDLs, elastin fibers which are deposited, etc. Build up results in the thickening of the walls.
Tuesday, July 18, 2006
Cow Heart pictures
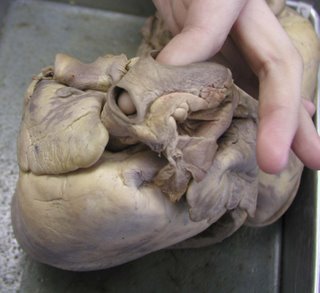 Worksheet for the Heart
Worksheet for the HeartStructures to ID:
Apex- The bottom of the heart.
Base- The top of the heart.
Pericardial Sac- The large thin flap on the base of the heart.
Epicardium (visceral Pericardium)- The outerside of the heart.
Myocardium- Inside the heart the thick looking pieces of steak.
Endocardium- The shiny gray stuff inside the heart.
Interventricular Groove- The line on the outside of the heart.
Left Atria- Towards the base of the heart on left side. It is located inside it between the two thick pieces of myocardium above chordea tendonae.
Right Atria- Towards the base of the heart on right side. It is located inside between skinny pieces of myocardium above chordea tendonae.
Left Ventricle- Towards apex of the heart on left side. It is located inside of the endocardium below the chordea tendonae.
Right Ventricle- Towards apex of the heart on right side. It is located inside of the endocardium below the chordea tendonae.
Tricuspid Valve- On the right side of the inside of the heart. Look for the chordea tendonae and it is the flap attached. It is in the endocardium.
Bicuspid Valve- On the left side of the inside of the heart. Look for the chordea tendonae and it is the flap attached to it. It is in the endocardium.
Pulmonary Semilunar Valve- It is located inside the pulmonary trunk.
Aortic Semilunar Valve- Inside the heart, it is the large hole located in the middle by the base. It comes out of the left ventricle.
Chordea Tendonae- The strings located inside the heart in the endocardium.
Papillary Muscle- Inside the heart, it is the bump where chordea tendonae attaches to the myocardium.
Interventricular Septum- Inside the heart, it is the myocardium in the middle that separates the two ventricles.
Superior Vena Cava- Outside of the heart on base and drains into right atrium. You should be able to stick finger through superior and inferior vena cava and your fingers should touch.
Inferior Vena Cava- Outside of the heart on base and drains into right atrium. You should be able to stick finger though superior and inferior vena cava and your fingers should touch.
Coronary Sinus- When you stick your finger through the superior vena cava, it is the thin spot.
Pulmonary Trunk (Artery)- It is located on the base of the heart. It resembles an elephant trunk.
Aorta- The large hole located on the base of the heart.
Pulmonary Veins- It is the large hole located on the base of the heart that drains into the left atria.
Coronary Artery- It is located on the base of the heart. It drains into the right atria, and is located directly on the side of the aorta.

 <------Vena Cavas (superior and inferior)
<------Vena Cavas (superior and inferior) 
Monday, July 17, 2006
Kidney model pictures



From the top Model (Thanks to Shawntell Smith again for typing these out)
Kidney ID:
Cortex- The lining around the kidney that looks like brown grains (28).
Pyramid- on the top under “vein like” structures (29).
Papilla- Tip of the pyramid towards center (30).
Column- Spaces between the pyramid.
Minor Calyx- Large white tube like structure (3D image).
Major Calyx- Where all the minor calyx goes into the middle (28).
Pelvis- Brown in the middle before ureter.
Ureter- Long tube coming out of bottom.
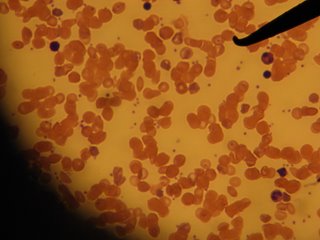
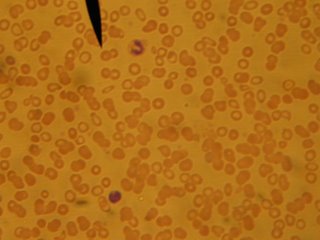 Monocyte/Lymphocyte
Monocyte/Lymphocyte